
Mental health in conflict: 'Occupation therapy' needed for Palestinians
The World Health Organization (WHO) has recognised mental health as an essential component of health since 1946.
Yet, around the world, mental wellbeing is an underfunded, under-resourced and largely misunderstood area of health provision. In extreme environments such as war, the detrimental impact on civilians' mental health is one of the most significant consequences.
Following recent events in Gaza and with the Israel-Palestine conflict now in its 70th year, Palestinians' need for adequate mental health services is a growing imperative.
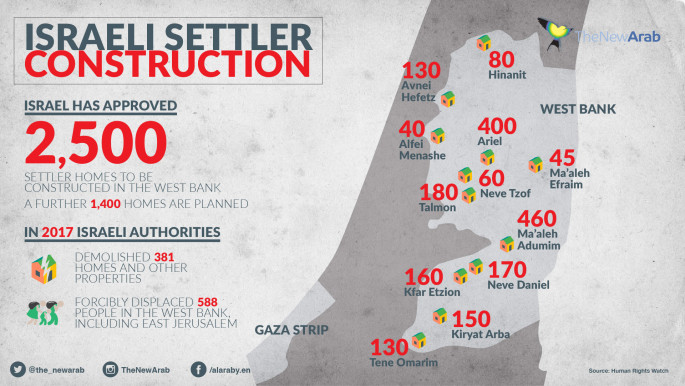
Over 50 years of occupation enforced by the Israeli military has exposed Palestinians to perpetual traumatic events including humiliation, imprisonment of youth, torture, house demolitions, land confiscation, movement restrictions and unemployment.
These routine human rights abuses are continual and pervasive. From apartheid road systems and checkpoints, to settlements and of course the wall, the psychological stress incurred by the occupation has left the population with one of the highest rates of mental health disorders in the Middle East.
 |
Trauma and anxiety are the most prominent effects of living in the occupied Palestinian territories |  |
Mental health workers across Palestine treat a variety of symptoms that have manifested as a result of the occupation. Israel has not fulfilled its international legal obligation as an occupier to implement its own mental health act, and the number of individual psychiatrists is limited. In the West Bank, there are just 22 trained professionals.
Unsurprisingly, trauma and anxiety are the most prominent effects of living in the occupied Palestinian territories (oPt), with women and children suffering disproportionately from mental health disorders, according to Chair of the Mental Health Unit at the Ministry of Health, Dr Samah Jabr.
As subjects of the Israeli occupation, Palestinians suffer multiple losses which often leads them to feel anguish and outrage. They are dispossessed of their belongings, and constant violence permeates every sphere of their lives alongside the terror of losing not only their children, but their homes and sometimes their mental health, too.
 |
|
The fragmentation of families due to fear, intimidation tactics and the removal of safe spaces is eroding the resilience which is integral to staying sane within the wall's confines.
Minds are being fractured, pushing the most vulnerable to suicide in numbers in never seen before. Despite suicide being condemned within Muslim societies, in Gaza recent statistics have indicated a surge in the number of people trying to take their life. Grassroots NGO We Are Not Numbers (WANN) noted 80 suicides per month in January and February 2016, an increase of 160 percent compared to previous years.
For Palestinians, trauma is not a post-event - it is growing up in a continued traumatic environment with no end in sight, and thus diagnoses such as post-traumatic stress disorder (PTSD) do not fit within the Palestinian context.
Read more: Mental health in Palestine among world's worst
Family therapist Charlotte Burke asserts that, "Individual diagnoses strip individuals of their context and in the special Palestinian case, vitally exclude the narratives of violation and injustice." Public Health professor at Birzeit University in the West Bank, Rita Giacaman, adds, "placing a medical label on social suffering does not help and can harm those violated by war".
Hunaida Iseed, Director of the Guidance and Training Centre for the Child and Family (GTC), believes the normalisation of Palestinians' experience of trauma in itself has negatively impacted the mental health field.
Iseed reports on the lack of commercial interest in funding trauma and PTSD research because of the extent it has become an accepted part of everyday life in Palestine.
Twitter Post
|
Mental health professionals depict the challenges they face within the unique, complex psycho-social context of the occupation, which psychotherapist Gwyn Daniel says "exerts control over, and intrudes into the most intimate aspects of human relationships". Consequently, the narrative of violation and injustice emerges as integral to the development of diagnosis.
The clinical director of Bethlehem's only mental hospital Dr Ivona Amleh for instance, is currently guiding a transition from a traditional medical model to one based more on recovery and empowerment, which incorporates the way power and oppression work; something she describes as 'occupation therapy'.
Dr Amleh asserts the need for mental health workers to be flexible, but shares the desire to shift towards specialising in order to provide better services.
Giacaman helpfully frames the ongoing conflict as a public health problem, which calls for an international response to work towards political conflict resolution and the realisation of human rights legislation.
After all, psychological wellbeing is an intrinsic aspect of the right to health; a point that was echoed by the UN Special Rapporteur for the Right to Health, who stated: "There can be no health without mental health and everyone is entitled to an environment that promotes health, well-being, and dignity."
Humanitarian aid and development models predominantly focus on addressing the basic physical needs of a vulnerable population. Societies have been slow to progress with mental health provision on a global-scale, and there is certainly a long road ahead before mental wellbeing is seen as important as physical.
In Palestine, the deep US funding cuts to the United Nations Relief and Works Agency (UNRWA) has left health care provision for Palestinians in dire straits. Psychological care must be integrated into primary health care, so that professionals can specialise in the areas needed to treat psychological effects of the occupation.
 |
Israel has not fulfilled its international legal obligation as an occupier to implement its own mental health act |  |
More international mental health professionals and institutions should partner with their Palestinian counterparts to help deliver effective care programmes.
Palestine's health sector requires sustainable development support from the international community so as to ensure that vital infrastructure and services such as local models of care are in place, to better respond to all health challenges of the population in need.
Anastasia Kyriacou works for AidEx, the world's leading organiser of international humanitarian aid and development events. She explores issues that instigate crucial sector dialogue among the community and beyond.
Follow her on Twitter: @AnastasiaKyria
Opinions expressed in this article remain those of the author, and do not necessarily represent those of The New Arab, its editorial board or staff.





 Follow the Middle East's top stories in English at The New Arab on Google News
Follow the Middle East's top stories in English at The New Arab on Google News


